|
ARTIFICIAL INTELLIGENCE IN RADIOLOGY; a French point of view
Jean-François Moreau, MD, AIHP, HyFacr
It is customary to oppose the practical intelligence of the animal which is the possibility of learning by weaving binary links typically illustrated by Pavlov's theory of conditioned reflexes, to the abstract and conceptual intelligence that only the brain human knows how to produce and consume. The definitions of artificial intelligence are more vague, inasmuch as it is only in the animal world that species have a brain whose functioning is still poorly understood, especially in the field of thought. They are therefore more technical than scientific. For the simple Larousse, it is the set of theories and techniques implemented in order to realize machines able to simulate the intelligence. For one of his parents, Marvin Minsky, it is the construction of computer programs that engage in tasks that are, for the moment, performed more satisfactorily by human beings because they require mental processes of high level such as: perceptual learning, memory organization and critical reasoning.
There is, on the one hand, the real existence of tools or machines that are already in the possession of the man who created them and that we call robots, in perpetual evolutive sophistication, but which remain under the domestication of their creator regardless of their gigantism or miniaturization. On the other hand, there are projects of all kinds that pretend not to serve the human race in a master-slave relationship, but to enslave the humans by producing either supermen self-managing to enslave them; if those supermen do not destroy the humans, they are tools so gigantic that, while remaining under the supposed human constraint, they are capable of inducing large-scale societal changes, both in professional life and in the relations of private order. In the latter field, science fiction writers have already invented myriad scenarios, all or almost all of which have proved their lack of chronological sense. Space exploration in 2001 as described by Stanley Kubrick and Arthur Clarke in 1968 with the appearance of a robot, HAL 9000, secreting artificial intelligence vector of a decisional independence, always appears as a sweet but formidable folly in 2018, even though supercomputers have managed to defeat the best human specialists in chess and go games. On the societal level, in 1949, George Orwell was similarly deceived in predicting the reign of Big Brother for 1984. The authors of Star War and Star Treck were better informed by locating their fiction at a distance of several centuries the time of their creation.
Is Laurent Alexandre wrong in announcing the death of radiologists for 2030? The case is important when we know that medical imaging is one of the most popular topics for new residents to choose from.
1. What is Medical Radiology in 2018?
1.1. The story
Let us first look at its past. Medical Radiology was born November 8, 1895, at the very moment when Wilhelm Conrad Röntgen, discovering a photographic plate impressed by an invisible light, radiographed the hand of his wife with what will become the X-rays. As a result, the Americans use willingly the word Rœngenology. What did he need? 1) electricity produced for the first time by Volta and then by Rumhkorff coils; 2) a photographic plate invented by Niepce then Daguerre; 3) a cathode tube of Crookes; all this was invented throughout the nineteenth century. In July 1900 took place the first unofficial international congress of electricity and medical radiology at the Paris Universal Exhibition. It was decided to call "Radiology" the discipline based on the use of X-rays for diagnostic and / or therapeutic purposes; the practitioners who indulged in it would be called "radiographes" in French or "radiographers" in English. Ten years later, in France, under the influence of Antoine Béclère and his school, the profession evolved with a schism between doctors who would call themselves "radiologists" and their nursing assistants who became "manipulateurs de. radiologie" in France while continuing to call them radiographers among the Anglo-Saxons. The training of radiologists more commonly called radiologists evolved in France with the creation in 1948 of a university chair and a national certificate of special studies of electro-radiology. In 1968 a major symposium was held at Enfants Malades in Paris, which led to the definition of Radiology as the third clinical discipline. Thereafter, was founded the Circle of Teachers in Radiology of France (CERF) intended to face the requirements of the Reformation Debré instituting full time university-hospital. In 1968, a profound reform was instituted which led to the formalization of the partial split of radiotherapy and total electrology save ultrasound. In 1983, the DES in radiology and medical imaging put an end to the major structural reforms announced by the introduction in 1975 of the concept of Medical Imaging and Interventional designed at Harvard University at Abrams department and UC San Francisco at Margulis department.
In 2018, the teaching of medical imaging is carried out during five years of residency to which one or two years of assistant professorship and / or attachments of variable duration are willingly added. Postgraduate education is compulsory. Hospital and university radiology is mainly full-time. Private radiology is practiced in groups of several radiologists more or less under-specialized in organ disciplines. Most of the French radiologist get retired in between 65 and 70-year-old. That means that the radiologist work at least during 40 years after graduation. There is no joblessness in radiology whether in private practice or in academics.
1.2. The patient
Since the origin of radiology, the PATIENT is the center of the radiodiagnosis chain as both a physical person defined by one or more body volumes to be studied and a legal person who must have accepted the realization of a prescribed examination for curative or preventive reasons. He or she is installed on a set of furniture that we will call hardware comprising a bed or a chair on which the applicant is lying or sitting or even standing in front of a source of X or ultrasonic and infrared radiations controlled by a functioning control equipment to electricity. Magnetic resonance is a separate instrument in that the patient is surrounded by a magnetic field in a noisy and uncomfortable environment. Isotope imaging for which products are ingested or injected is also a special case. Imaging examinations are divided into invasive, pathological (X-ray and isotope), or non-invasive (ultrasound, thermography) means. The number of patients benefiting from medical imaging is only growing and beautifying through the increase in the population and the emergence of new diseases, while others are disappearing. Imaging that has become functional applies to all volumes and organs of the human body by means of one or another of the radiative techniques. Among the major arguments, emerges the observation of the "geriatrization" of the population and its procession of more or less pathological disorders that modify the normal anatomy. It is not by the patient that artificial intelligence will pollute the chain of imaging. At most professionals will be embarrassed by the use of patient's educational databases for their own information, such as Doctissimo.
1.3. The radiological installation
The heavy structures of the hardware are constantly evolving under the influence of mechanical specialists but we do not see how the artificial intelligence drastically modify the shape of modern installations marked by the remote control of mobilizable parts. To make a practical comparison, in the 21st century, we always buy tables and chairs but, if styles evolve, the basic principle remains the same, except to adapt to the change of morphotypes of a higher population and heavier than the previous one or vice versa (ring size of CT and MRI). This is not the case for the software part of the mobile facilities of the diagnostic radiology room, which must adapt to the demand for automaticity. These facilities are heavy and uncomfortable and the number of physical accidents requires rationalization to protect both patients (falls) and personnel (irradiation). The imaging production chain goes through an image carrier and its storage. Both fluoroscopy and echoscopy are useful and indispensable for guiding human examination; they will evolve under the dependence of the progress of the video chain and the desire to compress the images will have long if not always to accommodate the desires of quality. Radiography always involves a means of capturing the image whether it is light-sensitive radiological films or paper media that may still need to be invented in the field of industry. Here again, advances in artificial intelligence do not threaten the profession of "radiographer" in the short term, even though chemistry has got the better of darkroom personnel. X-ray diagnosis in the 21st century is carried out in broad daylight or in electric light. In this respect, both diagnostic and other imaging techniques operate on mains electricity or on batteries for smaller portable ultrasound devices. It is hard to see what other energy source could be substituted for it. At most, we can expect artificial intelligence to optimize power consumption during long exams.
Indeed, it is in the field of the future of the medical image that the change takes place with the already remarkable PACS (Picture Archiving and Communication System) which combines both the storage capacity of the image on hard disks. and access to the on-demand image bank to remote peripheral screens. The future of cloud computing fits beautifully in this perspective, we will come back to it. Today, PACS claims too much memory for the storage of long video sequences and optical fiber systems need to be magnified to ensure higher data rates the day it is the totality of an examination that will be stored and no longer a simple selection of images made by the person responsible for archiving.
1.4. The radiological staff
Because the time has come when we must address the human resources that populate the path of medical imaging from prescription to its interpretation. There is first the prescriber; it is rarely the radiologist and even less the patient himself. Most often it is the attending physician that he / she is generalist or specialized. His education requires an apprenticeship of Bac + 12 years. What will be his level of computer learning to use in a practical and effective way the use of diagnostic methods initiated by artificial intelligence? Will he be more or less talented than his fellow radiologist? Still, the dialogue between these two characters will have to be more intense and better vertebrate than what we see today.
At the level of the imaging department, there are two characters who share the intellectual and technical roles according to institutions and personalities experienced or not. In principle it is up to the radiologist Bac + 12 to accept the prescription as it is or to modify it at best. He himself carries out less and less often the examination since the so-called special examinations of the radiology leave the remote table (barium explorations, UIV, encephalographs ...); the latter give way to computed tomodensitometric examinations (CT and MRI, mainly) whose protocols are often written in advance so that the practical realization is done by his "radiographer" independently of the radiologist. The transition from conventional radiology to medical imaging has only increased the need for radiologists.
Comes the moment to exhibit some caricatures of medical radiology professionals. For decades, the radiologist has been known to be a lazy, highly enriched, libidinous and fearful in his dealings with the patient. This is no longer the case today and, if he or she has no more worries to be made to earn a living honorably, it is at the cost of a job that deserves to be fairly rewarded the high cost of investment in the technical platform in 2018. Radiology has made such progress in the field of radiation protection that the black side of the profession of radiologist decimated by hematological malignancies is no longer an obstacle to the choice of the medical youth of a discipline that remains nevertheless vulnerable in its interventional side. In May 1968, some students at the Salpêtrière radiology school were campaigning for their profession to be elevated to the rank of American radiographers, and some of them did not hesitate to perform duties normally in the medical field only. At best, we blame the radiologists for not being sufficiently present with the patient, and the reproach they are made to be invisible is more than ever relevant.
2. Now let's take a closer look at what the future of artificial intelligence brings to healthcare medicine and diagnostic radiology.
For the President of General Electric Digital at the 2017 French Radiology Days, the sub-disciplines of medical imaging may be concerned by four sectors of artificial intelligence.
1. Jim Gray, Distinguished Turing Award winner, envisions "data science" as the fourth paradigm of science (empirical, theoretical, computerized, and now data-driven) and ensures that it would be shattered by the impact of technology information and the deluge of data (Big data). There is no doubt that medical imaging as a whole digitally participates in its own deluge. The G4 of the French radiology is strong to collect 500 000 radiological radiographs in its ecosystem, notwithstanding the fact that the usufruct of these documents belongs to the patient and cannot be pirated or sold; Nevertheless, the vulnerability of a totally automated system from acquisition to interpretation is due to several factors inherent in the ontology of the process itself: technical artifacts that undermine the quality of the examination, difficulty in defining the normal anatomy of structures examined and the limits between the normal and the pathological, the same volume of data to post on the cloud, "geriatrization" of the human model, complex pathological associations ... The rules of go as failures are known and invariable and we managed to imagine victorious strategies and tactics invented by the computer without giving the computer the right to change the board. This is not the case with medical reasoning and every human being is a separate entity.
2. An agile application is the result of a service-oriented architecture and an agile development paradigm. An agile application differs from the others in that it is loosely coupled to a basket of services with a decoupled orchestration layer, easily modifiable to fit the needs of work, and has a scalable architecture. Components in a loosely coupled system can be replaced by alternative implementations that provide the same service. As long as this obscure language is compatible with that of medicine, can we hope that one radiography is applied to another to distinguish the normal and the pathological? In this context, the control of the medical operator at the entrance and exit of the radiodiagnosis chain is essential.
3. Cloud Computing is an Information Technology paradigm that allows ubiquitous access to shared sets of configurable resource systems and high-level services that can be quickly provisioned with minimal management effort. often through the Internet. Cloud computing depends on sharing resources to achieve consistency and economies of scale similar to a public purpose. Who does not see the infinite expansion of PACS whose growth is limited only by the power of the mainframes and the speed of the optical fiber network that serves them? Unless we imagine that there is a robotic super radiologist there, there are only reasons to think that the two professions of radiologists and radiographers can coexist in the best comfort with an increase in their number and a considerable improvement. their respective qualities of professional life. Computer Assisted Doping (CAD) should be a liberating tool for the most contingent tasks.
4. Machine learning is a field of computer science that often uses statistical techniques to give computers the opportunity to learn (that is, gradually improve performance in a specific task with data without being explicitly programmed). The decision tree forest method: based on human-provided characteristics, the machine learning algorithm mounts a series of decision trees, tests them, and chooses the most efficient tree, selecting the most relevant parameters. relevant image to take into account. Here is the Deep Blue radiologist. When we know the scope of the medical field and consider the power of a field radiologist, we can see that the machine to learn is a progress of the third type that will take decades to become operational. ... if it ever succeeds. When one knows the difficulty of communicating between two languages spoken on the Planet and the risk of particularly serious misinterpretation in medicine of care or research which make of a patient a unique case of its kind, one can conjecture on the necessity to produce More and more educated radiologists lined with better structured X-ray machines to reliably feed the computers that make up the machine to learn.
5. How long will it take to homogenize the reference databanks when the morphotypes of a given population have to be integrated while France does not readily accept the racial dichotomy? Will a Vietnamese database be adapted to a group of Swedes from Stockholm, while the average Vietnamese morphotypes vary between Hanoi and Saigon? The computer scientist will not fail to answer that the Cluster Computing is here to solve the problem. Cluster analysis is an unsupervised learning method of creating, from a series of patient imagery, subgroups with similar characteristics, such as the Cochin experiment on a group of patients with Alzheimer's disease. scleroderma; here again the current PACS is only the embryo of a larger system, such as a beowulf. As for the support vector machine (SVM), it is based on a classifier algorithm which, based on human-provided characteristics, classifies the imagery into different subgroups; she suffers from the same uncertainties as the previous three. However, there is no doubt that man will have to continue to govern these products both at the entrance and the exit of the chain of the imagery.
6. The most disturbing figure of contemporary computing comes from the development of Deep Learning and its networks of artificial or convolutive neurons: computer neural networks imitating the architecture of human neurons (several inputs weighted information, an output value). It is from its sophistication that we can consider new HAL 9000. Who can say today that neuroscience have made such progress that they have demystified the anatomo-physiology of all the brain? Thought, in the world marked by Judeo-Christian ideology, remains a metaphysical domain. Dramatic for the future of our current societies would be the day when one could prove that this thought boils down to a problem of physico-chemistry a little more complicated than the others. The fate of radiology would be that of a human idol-breaking society embroiled in a generalized civilizational conflict that already exists in science fiction.
Conclusions
In their report commissioned by the Minister of Labor, Salima Benhamou and Daniel Janin do not fail to assert a contemporary reality: medical imaging professionals are particularly affected by the predictable generalization of automated image reading. But they remain reassuring on one point: whatever the field, the principle is always the same: the algorithms fed and driven by massive data (medical image recognition, results in medical research, etc.) are programmed to detect pathologies according to protocols predefined by the medical world. If we refer to the aforementioned science-fiction writers, their sense of foresight, their disaster scenarios have almost never happened in their lives (Kubrick died in 1999) or on the planned date (Orwell).
The radiodiagnostic machine, the day it will be invented and become operational, remains hypothetical in the more or less long term. It will long equip one or few privileged centers that will be responsible for making the evaluation that will require a lot of time because the hospital circuit is slow and, as for cohorts of patients, the bigger the more heterogeneous. If it is certain that in the very long term it could be envisaged that automated systems become commonplace throughout the practice of medical imaging, the national radiological staff would remain operational to supervise the medico-legal side of the radiographers' activity, kings of the technical service. Will radiologists be anything other than interventionists? This requires that the surgical discipline evolve towards more medical treatments and less bloody operations. In reality, it will be necessary to count on the effectiveness of the prophylaxis of the medical diseases and the preventive medicine of the diseases of the old age to upset the ordering of the three great clinical disciplines.
A RAVENSBRÜCK

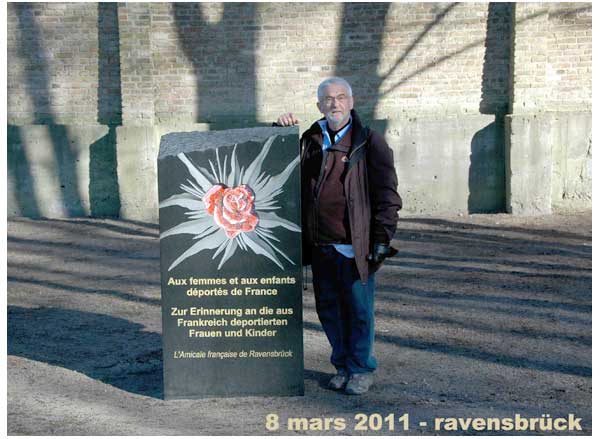
LA PHARMACIE DE MARGUERITTE CHABIRON
A VERDELAIS ETAIT DANS CET IMMEUBLE

LES RESISTANTES S'ENFUIRENT PAR LE JARDIN A PIC